The dirt in your backyard may hold the key to isolating cancerous tumors and to potential new treatments for a host of cancers.
University of Iowa researchers have found a gene in a soil-dwelling amoeba that functions similarly to the main tumor-fighting gene found in humans, called PTEN.
When healthy, PTEN suppresses tumor growth in humans. But the gene is prone to mutate, allowing cancerous cells to multiply and form tumors. PTEN mutations are believed to be involved in 40 percent of breast cancer cases, up to 70 percent of prostate cancer cases, and nearly half of all leukemia cases, according to a review of the literature by the UI researchers. Combined, more than 465,000 new cases of breast and prostate cancer have been documented in 2014, according to data from the American Cancer Society.
“If you look at tumors across the board—and that doesn’t mean just breast cancer or prostate cancer—you find that PTEN is the most generally mutated gene. And when you mutate PTEN in mice, you cause tumors,” says David Soll, biology professor and corresponding author on the study, published in the journal PLOS ONE.
While it’s unknown how to prevent PTEN mutations, the UI researchers became interested in finding out whether other human genes may substitute for PTEN, like a player coming off the bench when the star has been injured.
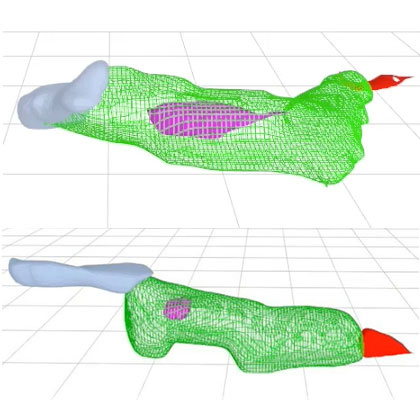
After some searching, the team found that an amoeba, Dictyostelium discoideum, has the gene ptenA, which mutates similarly to the human PTEN gene and causes behavioral defects in the cell. They also found a close relative of ptenA in the amoeba, which they called lpten that performs the same functions of ptenA, but to a lesser degree—a possible bench player in the amoeba’s genome.
The researchers hypothesized that ramping up the presence of lpten, making it the star on the court, could overcompensate for the mutated ptenA.
Soll and his team tested their hypothesis by placing lpten in a plasmid behind a powerful promoter designed to over-express the gene – essentially cranking up its power. They then introduced the super-charged lpten into a cell with the mutated ptenA gene. The researchers found that the over-expressed lpten gene fully overcompensated for all of the defects in the ptenA mutant.
If the hypothesis holds true for human cells, it could lead to a new way to treat cancer. The researchers want to look for a drug that would activate the promoter for one of PTEN’s close relative genes. Once a patient is diagnosed with cancer caused by a PTEN mutation, the patient could take the drug, over-express the PTEN bench player gene, and potentially stop cancer in its tracks, Soll says.
That could save many cancer patients from undergoing chemotherapy and radiation treatment for breast and other common cancers.
The finding has led the UI team to study other human genes that may be able to step in for the mutated PTEN gene and perform the same tumor-suppressing role. There are at least two close relatives of PTEN the researchers are currently studying.
“And nature might have put them there just for that, that’s the curious thing,” Soll explains. “Somewhere, there may be a backup system, what we call ‘redundancy,’ that might be the basis for better identifying tumors and possibly creating cancer-fighting drugs. You have another gene which might be able to step in for the broken gene to keep things normal, and that’s what we’re playing with here. It’s very sophisticated.”
Daniel Lusche of the University of Iowa is the first author on the paper. Contributing authors on the study include Deborah Wessels, Nicole Richardson, Kanoe Russell, Brett Hanson, Benjamin Soll, and Benjamin Lin, all working in the Monoclonal Antibody Research Institute in the Biology Department at Iowa.
The Developmental Studies Hybridoma Bank, a national resource created by the National Institutes of Health and housed at the University of Iowa, supported the study.