Robert Mullins, a University of Iowa associate professor of ophthalmology and visual sciences and his colleagues have acquired one of the largest collections of donated eye and eye tissue samples in the world, an invaluable resource for studying both common and rare eye diseases. Since 2004, the team have collected approximately 1,400 eyes for research and transplantation.
Because the anatomy of the human retina is unique, the research being done with donated eyes cannot be easily replicated in animal models. Samples from the Iowa Lions Eye Bank are also sent to investigators around the world to aid in various research projects.

“The people in this community are incredibly generous, and Iowa has one of the highest percentages of identified organ donors,” Mullins says. “Especially those people with rare eye diseases; they’re very eager to help out by donating.”
Collecting corneas for transplantation is a major component of the eye bank’s mission, which directly improves the lives of cornea recipients. But not all donated eyes are suitable for transplantation. When that happens, those eyes are used for research to understand the aging process and biology behind eye diseases, including macular degeneration, retinitis pigmentosa, glaucoma, Fuchs corneal dystrophy, and others.
Did you know?
Last year at UI Hospitals and Clinics, 40 donors gifted their eyes to research, and 85 cornea donors gave the gift of sight to 111 recipients in Iowa, the U.S., and around the world.
More than 1,800,000 donors are registered with the Iowa Donor Network. Register at iowadonorregistry.org.
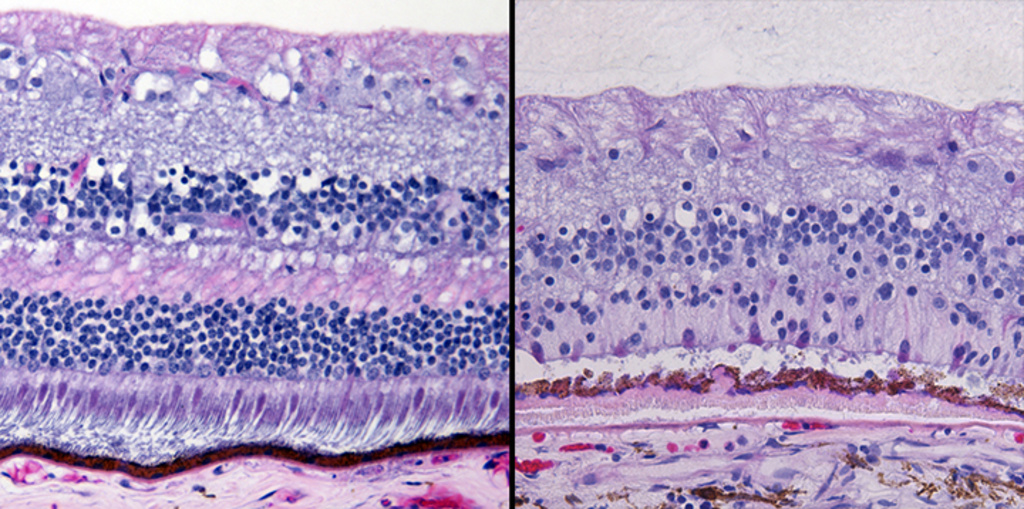
Lately, the UI research team has been using donor eyes to try to understand how and why specific genes are turned on and off. Macular degeneration, for example, damages the central part of the retina (the macula), such that focused vision is impaired, but peripheral vision is normal. Retinitis pigmentosa, however, leaves the macula alone, but causes degeneration in the periphery. Researchers are hoping to figure out why some diseases destroy these different areas of the retina and hope to better understand the molecular differences of those regions.
Other research projects are focused on stopping or slowing down the progression of macular degeneration. The first cells to succumb to the disease are in the layer beneath the retina—the retinal pigmented epithelium. Previous experimental therapies have tried to fix those cells.
“But what we found when we looked at eyes with macular degeneration,” Mullins says, “is that the loss of blood vessels beneath that layer actually happens first, so we first need to figure out how to rescue or replace those dying blood vessels.”
Stem cells provide a promising possibility for replacing those dead blood vessels, according to Mullins.
“What we’re really hoping is to be able to make the remaining healthy cells resistant to any future damage. And if it’s bad enough, to deliver new cells from the patient to repopulate the damaged cells with healthy cells,” he explains.
Video courtesy of UI Health Care Marketing and Communication.
“It can be difficult when families are confronted with the decision about organ and tissue donation. But I want to be sure to thank the patients and their families,” Mullins says.
He also points out the tireless efforts of the staff at the eye bank and the people who go out in the middle of the night to collect and preserve samples to continue fueling this important research.
To read several related stories, see Taking the long view: Triathlete teams with UI researchers on blinding eye disease, and A blind man's daily journey.
Editor's Note: This story was originally posted in The Loop, an interactive online employee newsletter for UI Health Care faculty, staff, students, and volunteers.