When U.S. Marine Cpl. Michael Meyer woke up at University of Iowa Hospitals and Clinics in early May, he remembers being told, “You’re in Iowa.”
His first thoughts were “Where?” and “Why?”

Iowa, Meyer would find out, was a key destination on a road to recovery from severe respiratory failure that nearly took his life. How he ultimately came to the UI is a story of personal strength, family devotion, and the collaboration between UI Heart and Vascular Center specialists and medical personnel from the U.S. Army, Navy, and Air Force.
For the 23-year-old Meyer—a bright, dedicated, and physically fit Marine from Florida who could easily finish a 15-mile run while he was stationed at Camp Schwab on the island of Okinawa, Japan—what had begun as a cough in early March quickly progressed to a serious lung infection. During a training mission on March 13, Meyer felt winded to the point where he could barely stand. Immediately he was evacuated to U.S. Naval Hospital Okinawa.
“I sat down in a wheelchair, and they started taking off my boots. The next thing I know, I was being sedated,” Meyer recalls. “I went from an oxygen mask to anesthesia. I don’t remember a whole lot after that.”
Despite being placed on a ventilator (breathing machine) and receiving powerful antifungal and antibiotic medications, Meyer’s health grew worse. His condition was critical, according to his mother, Laurie Meyer Cox, of Pensacola, Fla. The Marine Corps had contacted Cox and Meyer’s father after the Marine was hospitalized and arranged travel visas and transportation for the parents to be at their son’s bedside.
“Being a nurse myself, I knew what the vent settings meant,” Cox says. “Michael needed a lot of oxygen. He was fighting for his life, yet he continued to get sicker and sicker.”
Several days later, Meyer “blew a hole in his lung,” Cox says, referring to a pneumothorax, or collapsed lung. It was the first of several serious complications that had the hospital staff working around the clock to keep Meyer alive.
For the medical team, it became clear that Meyer needed specialized support technology known as ECMO, or extracorporeal membrane oxygenation. Traditionally used to support newborn or premature babies, an ECMO system does the work of the heart and lungs by circulating blood through an artificial lung back into the bloodstream—removing carbon dioxide and adding oxygen and giving the patient time for the lungs and heart to “rest” and heal. For Meyer, ECMO was his best, and perhaps only, chance to allow his lungs to regain their strength.
“We were told on a Friday that we were going to lose Michael if we didn’t get him off the island by Monday,” Cox recalls.
From Japan to Hawaii
Working against the clock, Cmdr. Joon S. Yun, director of medical services at U.S. Naval Hospital Okinawa, called the U.S. Air Force in the Pacific to help coordinate and make other contacts necessary to pull off a life-saving flight. U.S. Army Lt. Col. Erik Osborn, a pulmonologist and intensive care specialist at Tripler Army Medical Center in Honolulu, Hawaii, assembled a 12-person ECMO transport team composed of medical specialists, nurses, and technologists from Tripler, the Pacific Air Force’s Critical Care Air Transport unit, and the Hanuola ECMO program at Kapi’olani Women’s and Children’s Medical Center in Hawaii. In less than 24 hours, the team was airborne for Okinawa.
Background: More about ECMOWhy Iowa?See the video...
ECMO, or extracorporeal membrane oxygenation, provides cardiac and respiratory support for patients whose heart and lungs can no longer function adequately on their own. Developed from cardiopulmonary bypass technologies first used to facilitate open-heart surgery in the 1950s, ECMO became a clinical reality in the 1970s.
In order to initiate ECMO, a surgeon inserts tubes into the patient’s large blood vessels. With the help of blood thinners to prevent clotting, the system pumps blood from the patient to the membrane oxygenator, or artificial lung, and returns it back into the patient. The membrane oxygenator removes carbon dioxide from the blood and rejuvenates it with oxygen, exactly as healthy lungs would do.
While ECMO programs for babies and pediatric patients are relatively common, UI Hospitals and Clinics is home to one of the few centers that specialize in adult patients, notes William Lynch, MD, director of the ECMO program at UI Heart and Vascular Center.
“Today there are less than 30 centers in the U.S. that do a meaningful number of adult ECMO cases,” Lynch says. “It takes commitment to establish and support an adult program. ECMO is not easy to do—it’s time-consuming and requires a lot of resources, education, and collaboration. Over the past few years we’ve established a solid program for adults as well as children—our clinical skills are very good, and we’ve had great results compared to registries that track these patients.”
Between 25 and 30 patients receive ECMO treatment at UI Heart and Vascular Center each year; half of these are adults. Those numbers, along with a recognized education and ECMO simulation program for physicians, nurses, and trainees, has led to a system of care with a reputation that’s known beyond Iowa. Lynch and his colleagues receive calls from hospitals and other ECMO programs around the country and the world.
Lynch notes that several factors—improvements in ECMO technology over the past two decades, the emergence of H1N1 influenza pandemic in 2009, and research demonstrating improved success rates compared to other support strategies for respiratory failure—has led to renewed and increased interest in ECMO. As the technology continues to advance and more clinical studies are done over the next 10 years, the use of ECMO for adult respiratory patients likely will increase dramatically.
“Historically for adults, ECMO was offered for five to 10 days, and if the lungs didn’t get better after that period of time, it was common to discontinue care,” he says. “But researchers and clinicians are now recognizing that if you support these patients long enough—even 30 days or more—the lungs will get better. You have to be willing to wait it out, and that means being able to handle the logistics and having well-trained people who understand the technology and can do it correctly and safely.”
Click here to hear Michael and Laurie recount the story of Michael's illness and recovery.
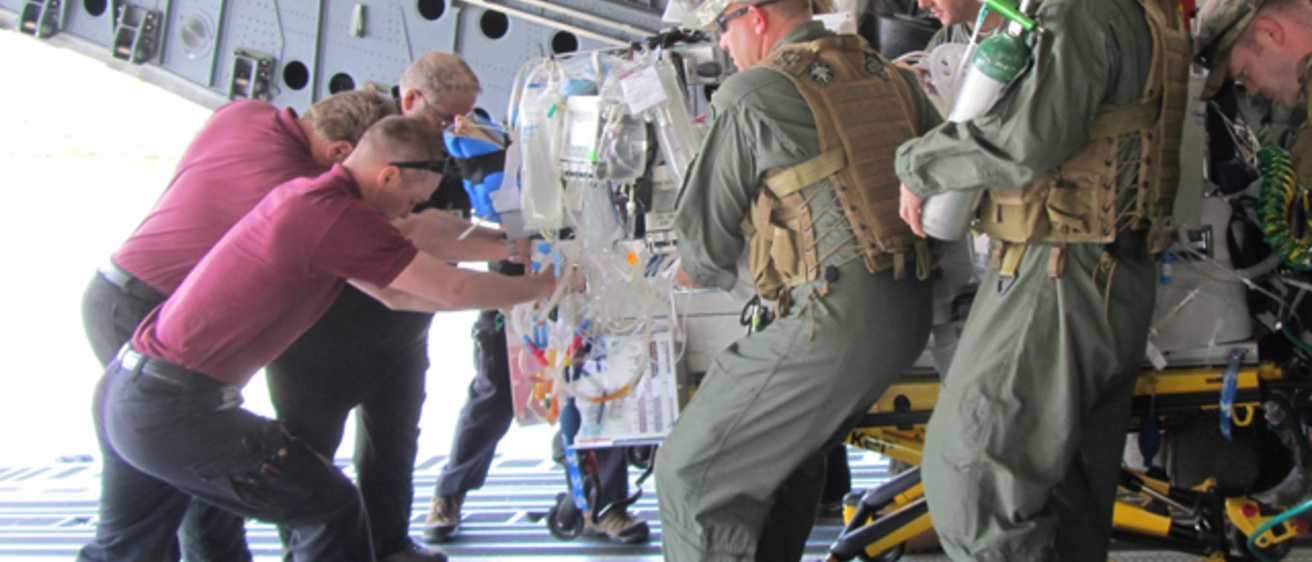
As soon as they arrived on March 26, the team went to work. Once Meyer was connected to the ECMO system and stable enough for transport, the ECMO team and hospital staff began the complex process of getting him to Kadena Air Base, where he would board an Air Force C-17 cargo jet to take him on the 10-hour flight back to Hawaii.
It’s worth noting that although long-distance transfers of patients on ECMO had been done with severely ill babies and with war casualties in Iraq and Afghanistan to the Army Medical Center in Germany, Meyer’s case was the first time in the entire western Pacific that the ECMO transfer procedure had been done with an adult patient. The flight from Okinawa to Hawaii was the longest adult ECMO transport in history.
Despite Meyer’s critical condition—and the inherent challenges in a long-range flight involving complex medical equipment, tubes and instruments, generators, blood products, medicines, IVs, monitors, and more—the transport to Hawaii went smoothly. The ECMO team, and Meyer’s mother, Laurie, remained by his side throughout the entire flight.
Meyer continued to struggle at Tripler Army Medical Center, however. Besides not being able to breathe on his own, he had bleeding issues related to the chest tubes inserted after his lung collapsed and the blood-thinning medications necessary for ECMO treatment. Meyer’s course was especially challenging since ECMO was initiated later than usual (11 days after being placed on a ventilator) and he had two reasons for life-threatening respiratory failure (an infection and a large hole in his right lung). Meyer also had kidney problems from the antifungal drugs and other complications.
“We soon realized that Cpl. Meyer would need ECMO for more than a couple of weeks, and we simply didn’t have the resources to handle such a long ECMO run,” Osborn says. “There aren’t many centers in the U.S. that are equipped to provide high-quality, long-term ECMO for adults. What Mike needed was the next level of care, so I called Dr. Lynch at the University of Iowa.”
In fact, Osborn had been in daily contact with William Lynch, MD, clinical associate professor of cardiothoracic surgery and director of the ECMO program at UI Heart Vascular Center, since first learning about Meyer’s case. Osborn and Lynch had previously worked together treating other ECMO patients, and both are active in ELSO (Extracorporeal Life Support Organization), the international ECMO group for which Lynch is an instructor and chairman.
“ECMO has been a standard of care in neonates for almost 30 years, but it’s only emerged as an acceptable rescue therapy in adults over the past decade,” Osborn continues. “We, and Cpl. Meyer’s parents, wanted to go all the way and support him with ECMO for as long as possible. We knew Dr. Lynch and his team had the knowledge, the experience, and the system in place for a case like this.”
Next stop: UI Hospitals and Clinics
On April 1, after one week at Tripler, Meyer—still connected to ECMO and a ventilator and accompanied by the medical team and his mother—was loaded back onto an Air Force C-17 for the nine-hour flight to the Eastern Iowa Airport in Cedar Rapids. As with the Okinawa-to-Hawaii transport, the flight to Iowa required precision and focus from the medical team to ensure that Meyer remained stabilized during the flight and that the ECMO system, intravenous drips, and other key pieces of equipment were working properly. Upon their arrival, the transport team worked closely with local emergency medical services personnel to deliver the patient to UI Hospitals and Clinics safely.
When Meyer arrived at the UI, “our immediate issues centered on bleeding caused by the chest tubes, kidney function, and the ongoing lung support that ECMO was providing,” Lynch says. “Brain damage or other neurological issues also was a concern. So the first several days were spent focusing on these issues and then liberating the sedation and other medications that were necessary to safely get him here.”
With each day, Meyer slowly made progress toward recovery. His brain function was good—once he awoke from the sedation, he was able to understand and respond to the medical team and his family. Lynch did chest surgery to evacuate and control the bleeding and also performed a tracheostomy (a surgically made hole into the trachea, or windpipe) to make Meyer more comfortable while he was on a ventilator.
Also, while still connected to ECMO, Meyer began physical therapy—getting to his feet or moving to a chair, for example—to help him regain strength and counter the effects of being bed-ridden for weeks. Slowly over time, he was able to breathe on his own for a few minutes and take short walks outside his hospital room.
On May 1, after more than a month on ECMO, Meyer was taken off the machine; the ventilator was removed a week later. He was still weak—Meyer had lost 40 pounds from his 175-pound frame since his illness began—but the fact that he was alive was remarkable. Finally, in late June, Meyer was discharged to go home to Florida, where he has since begun physical therapy and rehabilitation. His future with the Marines is uncertain, but Meyer admits he’s not looking that far ahead.
“Just to get back to healthy again—that’s really the only goal I have right now,” he says.
Other than a brief trip home during Meyer’s stay at the UI, Laurie Meyer Cox was at her son’s bedside every day. Looking back, she’s amazed at the dedication and the coordinated, sustained effort that saved his life.
“At every step, we were able to get Michael to the next level of care that he needed, and that wouldn’t have been possible without the military branches working together,” Cox says. “I mean, here’s a Marine who went to a Navy hospital, was transferred by the Air Force to an Army hospital, and then transferred again to Iowa. They were able to overcome every obstacle in Michael’s care as a team.
“And the care Michael received at the University of Iowa was phenomenal. Even during the dark days and hard times, everyone was calm, everyone was professional. I would say repeatedly every day, ‘It’s another great day in Iowa.’ We have so much to be thankful for. This has been an incredible journey and we’re just glad to be on the other side.”