Chances are you won’t know you’ve got a staph infection until the test results come in, days after the symptoms first appear. But what if your physician could identify the infection much more quickly and without having to take a biopsy and ship it off for analysis?
Researchers at the University of Iowa may have found a way. The team has created a noninvasive chemical probe that detects a common species of staph bacteria in the body. The probe ingeniously takes advantage of staph’s propensity to slash and tear at DNA, activating a beacon of sorts that lets doctors know where the bacteria are wreaking havoc.
“We’ve come up with a new way to detect staph bacteria that takes less time than current diagnostic approaches,” says James McNamara, assistant professor in internal medicine at the UI and the corresponding author of the paper published Feb. 2 in Nature Medicine. “It builds on technology that’s been around a long time, but with an important twist that allows our probe to be more specific and to last longer.”

The UI-developed probe targets Staphylococcus aureus, a species of staph bacteria common in hospitals and found in the general public as well. The bacteria causes skin infections, can spread to the joints and bones and can be fatal, particularly to those with weakened immune systems.
“Every year in the U.S., half a million people become infected by S.aureus bacteria, and 20,000 of those who become infected die,” adds Frank Hernandez, a post-doctoral researcher at the UI and first author on the paper. “We believe that we are significantly improving the actual methods for detecting bacteria with a simple approach, which we expect to be cheap, fast and reliable.“
What makes staph especially troublesome is doctors don’t know the bacteria are in the body until they get the biopsy results, which usually takes days. “They’re flying blind, so to speak,” McNamara says. “It’s the state of medicine at this time.”
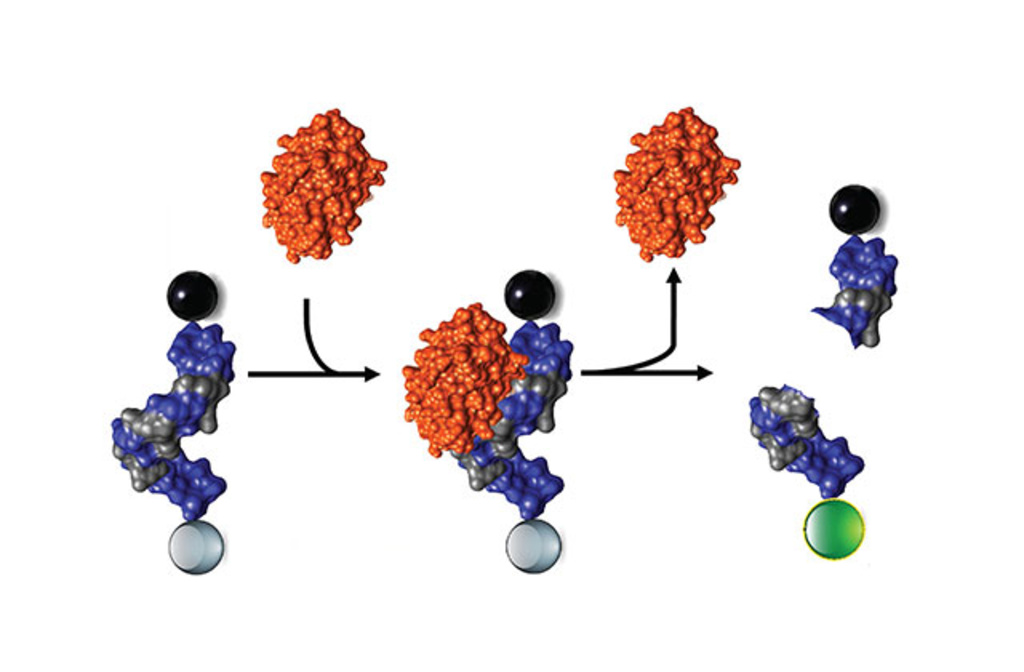
The UI team created a synthetic probe with two unique features. On one end is a molecule that gives off light under certain conditions. On the other end is another molecule that blocks that light. In other words, the particle, as designed, cancels itself out, leaving itself undetectable inside the body.
This is important due to what staph bacteria will do to the particle. In tests, nucleases (or enzymes) produced by the staph bacteria cleave the particles, like a warrior wielding a sword. (Why it does this is unclear, but scientists believe it’s a clever way for staph, which can’t move by itself, to spread beyond the molasses-like environment created when DNA leaks from infected, dying cells.) In any event, when staph cleaves the probe, it separates the light-emitting molecule from the light-blocking molecule, which then drifts too far away to block light. And, so with the right equipment, doctors would be able to see the light-emitting molecules and know that staph are raging there.
Outfitting such particles is not altogether new, but McNamara and his colleagues produced a probe that lasts longer—by several hours longer for certain types.
“We designed a tracking system that specifically identifies bacterial body localization in less than one hour,” says Hernandez, a Colombian who for years has been working on probes to detect harmful bacteria.
Just as important, the UI probe has been chemically modified so that it’s shredded only by the staph bacteria’s nuclease and not by a nuclease secreted by normal, healthy cells. The team further tested the probe in mice and human serum and report that it performed as expected.
“That’s the central idea, the underlying concept of our approach,” says McNamara, whose primary appointment is in the Carver College of Medicine. “If the probe gets cleaved by serum nucleases, then our probe would be lit up all over the bloodstream. But since it’s split only by staph nucleases, then we can pinpoint where the staph bacteria are active.”
The team, which applied in fall 2012 for a final U.S. patent for the probe, plans to refine the probe, so it can be detected deeper in the body and to test its performance with catheter infections, according to McNamara.
McNamara acknowledges previous research by Arthur Arnone, UI professor emeritus in biochemistry, who was the first to define the structure of the S. aureus nuclease.
Contributing authors from the UI include Michael Olson, Luiza Hernandez, David Meyerholz, Daniel Thedens, Alexander Horswill. Lingyan Huang, Kristy Powers, and Mark Behlke from Integrated DNA Technologies in Coralville, Iowa also contributed to the study.
The National Institutes of Health (grant numbers AI 083211 and R21 AI 101391) funded the research. Hernandez is supported through a fellowship from the American Heart Association.